Household Catastrophic Health Expenditure Due To Tuberculosis: Analysis From Particularly Vulnerable Tribal Group, Central India
M Muniyandi, VG Rao, Jyothi Bhat, Rajiv Yadav and RK Sharma
DOI10.21767/2471-8521.100009
M Muniyandi*, VG Rao, Jyothi Bhat, Rajiv Yadav and RK Sharma
National Institute for Research in Tribal Health (ICMR), Jabalpur, India
- *Corresponding Author:
- M Muniyandi
National Institute for Research in Tribal Health (ICMR)
Nagpur Road, P.O, Garha, Jabalpur 482 003
Madhya Pradesh, India
Tel: +91 761 2370800
Fax: +91 761 2672835
E-mail: mmuniyandi@yahoo.com
Received date: 23 October 15, 2015; Accepted date: December 11, 2015; Published date: December 20, 2015
Citation: Muniyandi M, et al. Household Catastrophic Health Expenditure due to Tuberculosis: Analysis from Particularly Vulnerable Tribal Group, Central India. Med Mycol Open Access. 2015, 2:9. doi: 10.21767/2471-8521.100009
Copyright: © 2015 Muniyandi M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Tuberculosis (TB) is disproportionately affects the most economically disadvantaged strata of society. Many studies have assessed the association between poverty and TB, but only a few have assessed the direct financial burden TB treatment and care can place on households. Patient costs can be catastrophic health expenditure for TB affected households in particularly vulnerable tribal groups (PVTGs). A survey of pulmonary tuberculosis (PTB) was carried out in Saharia dominated Pohri block of Shivpuri district of Madhya Pradesh state in central India during the period 2013 to 2014. Of 9964 surveyed, 280 PTB cases identified formed the study population for the present study. Among 280 TB patients identified, 220 (79%) cases interviewed at their residence by trained field investigators after obtaining written informed consent. This study demonstrates the economic burden in terms of direct, indirect and total costs for both diagnosis and treatment. In our sample, majority getting treatment free of costs and those who incurred costs, they faced catastrophic TB care expenditure amounted to 10%, which is the proportion of various costs in relation to annual family income. TB is a major cause of impoverishment, as it puts a heavy burden on the family budget, which can force families to absolute poverty. Our results suggest that policies to decrease direct and indirect TB patient costs are urgently needed to prevent chances of catastrophic payments to PVTGs. Also a high priority should be given to research that focuses on economic effects in different kind, in different time, in particular, among low-income
Keywords
Tuberculosis; Economic impact; Catastrophic health expenditure; Poverty; Vulnerable population; Tribal group; India
Introduction
Health is one of the most important components of an effective poverty reduction strategy. Since health can increase productivity and household income, while poor health is likely to reduce output. Health improvements can provide poor households with the opportunity to escape poverty. However, use of health services is critical with a view to out-of-pocket (OOP) payments and it is the primary means of financing healthcare in many low-income Asian countries. OOP payments can results in households facing catastrophic health spending, lead to impoverishment, and financial risk protection measures are missing. Globally it is estimated that 150 million people suffer financial catastrophe each year due to health care payments and about 100 million are pushed into poverty because of OOP payments [1]. Protecting households from catastrophic health care costs is a desirable objective of health systems worldwide. The WHO call for universal health coverage emphasized the need to protect households from catastrophic medical expenses and impoverishment arising from seeking health care.
TB is an airborne infectious disease thought to infect almost one-third of the world's population. It commonly manifests as an infection of the lungs, usually with symptoms of coughing, weight loss and other constitutional symptoms. Individuals suffering from TB are often in their economically most productive age, which poses a significant economic burden on the household. Poor people have longer pathways to care and costs of accessing care are generally higher before than after diagnosis [2,3]. Evidence indicates that the damaging effects of TB are catastrophic to those who were relatively poor or marginalized before being infected with TB and subsequently pushes the income insolvent into poverty [4-6]. TB is a chronic disease requiring long duration (6-8 months) of treatment make the poor patients vulnerable, deprived and locks them in the poverty stricken condition [2,7]. Thus poverty and TB are locked in a vicious cycle, as one triggers the other. The directly observed treatment short course (DOTS) strategy is costeffective strategy both from provider and patient point of view against historical controls [8-12]. Key components of the DOTS is that patient is VIP (very important person), programme’s responsibility to cure them, each dose of anti-tuberculosis drugs should be administered to patients under the supervision of a DOT provider, either from the community or the health system, according to patient’s convenience, so that patients do not lose wages or incur transportation charges for treatment under the programme [13]. This strategy has been successful in reducing costs to patients, death rates 38/100000/per year in 1990 to 22/100000/per year in 2012 and increasing cure rates [14].
TB disproportionately affects the poor people and TB control programs therefore need to ensure that the economically and socially disadvantaged groups do not face barriers that keep them from seeking treatment. It was estimated that on an average, 3-4 months of work time are lost if an adult has TB, resulting in a loss of about 20%-30% of annual household income [3]. Relative costs for poor people as a percentage of their income is much higher than for non-poor patients, although aggregate real costs may be smaller [2]. As per Government of India Census 2011, India has a high concentration of indigenous tribal population constitutes 8.6% of the total population of the country. As many as 705 groups are identified as tribal across 30 states, 75 have been identified as particularly vulnerable tribal groups (PVTGs) and Saharia population in Madhya Pradesh is one among them. It was reported that high magnitude of TB among Saharia tribe (1518/100000) [15,16]. Any development programme initiated by Government Of India will take time to reach this segment with limited access to health care services due to isolation, low social status and weaker economic position. TB programme therefore need to ensure that the economically and socially disadvantaged groups do not face barriers that keep them from seeking treatment. Hence, studies on patient costs towards costs of accessing care before than after diagnosis are needed particularly among most vulnerable population. Therefore, we undertook a study to estimate the OOP expenditure (diagnosis and treatment) to Saharia PVTG on account of TB in India. In this paper, we present the results of our study in terms catastrophic health spending through direct medical, direct non-medical, indirect and total costs.
Methodology
Setting
The areas of habitation of Saharia population in Madhya Pradesh are Gwalior, Datia, Morena, Sheopur, Bhind, Shivpuri, Ashoknagar and Guna. This study was carried out in Shivpuri district considering the operational feasibility, rapport with community and willingness to support by district authorities. Community survey done among Saharias in these areas by National Institute for Research in Tribal Health (NIRTH) showed most of them were labourers and annual family income of Rs<10000. Majority was illiterate and they resided in kaccha houses/huts with no separate kitchen in houses.
Study area
A survey of pulmonary tuberculosis (PTB) was carried out in Saharia dominated Pohri block of Shivpuri district in Chambal Division of Madhya Pradesh during the period 2013 to 2014. The same area was selected for this study.
Study population
All individuals aged 15 years and above were screened for PTB by chest symptoms such as persistent cough for two weeks or more; chest pain for one month or more; fever for one month or more; and haemoptysis anytime in last 6 months. All symptomatics were investigated by sputum smear and culture examinations. All the bacillary cases detected from the survey formed the study population.
Data collection
Semi-structured, pre-coded, pre-tested questionnaire was used for data collection. The interviews were conducted at home in their local language (Hindi) by trained field investigators. The interview included household identification, demographic and socio-economic characteristics of respondents. In addition, data on various costs such as direct medical (fees, investigations, drugs); non-medical costs like travel and special food for patient and escort; and indirect costs due to work absenteeism and loss of income were also collected. The interview team was supervised by trained supervisors during data collection. Costs data were validated throughout the interview by repeated questioning and cross checked with the prevailing rates of doctor’s consultation fees, costs for investigations, and market price of drugs, medical bills wherever possible. All the filled forms sent to NIRTH to check for correctness and completeness, any incomplete forms sent back to field for corrections within 15 days.
Definitions used
Information about the costs was ascertain for full course of treatment of newly diagnosed pulmonary TB patients, classified as category one as per revised national tuberculosis control programme (RNTCP) guidelines. All costs were calculated period starting from the moment of onset of symptoms up to the completion of treatment which included cost for diagnosis and treatment. Total cost covered expenditure incurred under direct and indirect costs [17] for 6 months-8 months of treatment. All these patients had taken treatment in government hospitals where the investigations and the medicines were offered free of costs for TB treatment. However they had to spend for travel etc., the distribution of costs is uneven and we are of the opinion that this variation is expected from all economic data such as income and expenditure. Further we classified the costs into nil cost, and for those who incurred expenditures mean, standard deviation, median, and range was calculated. The cost was calculated in terms of Indian rupees and US dollars (exchange rate at the time of study: $1 US=Rs.60).
Direct patient costs: Direct patient costs included all OOP expenditures of patients that were attributable to their illness. Consultation fees and money spent on investigations and drugs were classified as medical costs. Money spent for transportation to health facilities and costs of food bought during waiting time at the health facility. These costs were assessed for both patients as well as persons accompanying them and classified as non-medical costs.
Indirect patient costs: Indirect patient costs refer to the costs associated with work absenteeism and loss of wages due to illness. These costs included visits to the health facilities and hospitalization as well as other work absenteeism and loss of wages due to the inability to work as a result of the illness. In order to quantify the magnitude of loss of income, number of days absent for work was multiplied by the estimated income of the patient and escort.
Total cost: Total cost included both direct and indirect costs covering the expenditures incurred for pre-treatment and during treatment period.
Catastrophic spending: There is no single accepted definition of catastrophic spending. Some studies assess payments in relation to the budget share [18,19], while others argue that catastrophic spending should be measured in relation to capacity to pay (i.e. household expenditure net of food spending) [20]. Nonetheless, all measures suggest that when households spend a large proportion of their budget on health care, they often forego other goods and services, which can have negative implications for living standards [21]. Often, the choice of the threshold is arbitrary but two commonly used ones are 10% of total income or 40% of non-food income (referred to as capacity to pay) [22]. To capture the burden on these households, a measure of the depth of poverty is needed [23].
Data management and analysis
Data entry was done by using the census and survey processing system (CSPro) software package version 5.0 Data entry format was developed with logical expressions and conditional statements used to minimize the errors in data entry. Data were analyzed using statistical package for social sciences (SPSS/PC version 20.0; SPSS Inc., Chicago, IL, USA). In univariate analysis, average (mean) costs were compared and independent t-test was used to compare their demographic and socioeconomic characteristics and tested for statistical significance. A p-value 0<0.05 was considered as statistically significant. We reported mean values to allow comparison with other published cost estimates.
Human subject protection
This study was approved by the technical advisory committee and Institutional Ethics Committee of NIRTH, ICMR. We interviewed respondents after obtaining voluntary, written informed consent.
Results
Source of intake and coverage of study population
During the period 2013 to 2014, all individuals aged 15 years and above were screened for PTB by chest symptoms such as persistent cough for two weeks or more; chest pain for one month or more; fever for one month or more; and haemoptysis anytime in last 6 months. All symptomatics were investigated by sputum smear and culture examinations. Saharia tribal population surveyed was 9964 and 280 TB cases identified was the source for the present study. Among 280 TB patients identified, 60 (21%) could not be interviewed, 42 moved temporarily, and 18 had expired. The remaining 220 (79%) cases interviewed at their residence (Figure 1).
Profile of study population
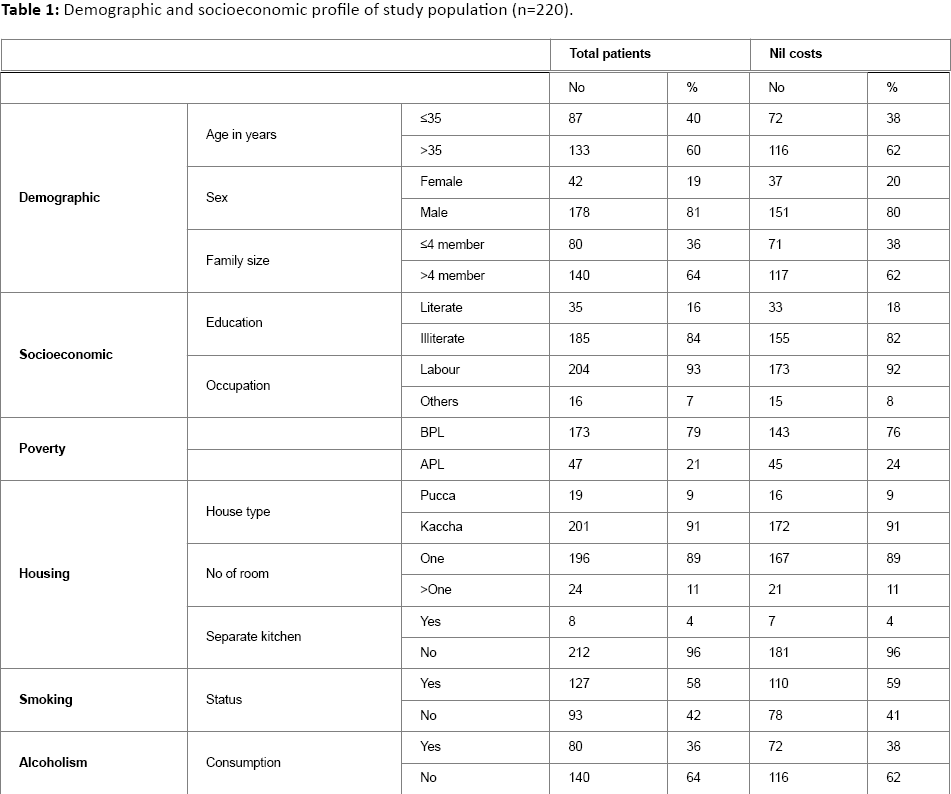
Majority of the patients (81%) belonged to 35 years age group and above. The study group included 178 (81%) males and females 42 (19%). Most of the patients 185 (84%) were illiterates and 204 (93%) were working as labour. Based on monthly per-capita income (definition of Planning Commission, Government of India; those per capita income Rs<660), patients were grouped into below poverty line and above poverty line. It was found that majority of patients were living below the poverty line. With reference to their living standards, 201 (91%) living in kaccha houses, 196 (89%) were single room houses; 212 (96%) didn’t have separate kitchen and were cooking in sleeping room (Table 1). The life style characteristics of patients were 58% smokers and 36% alcohol consumers.
Overall patient costs
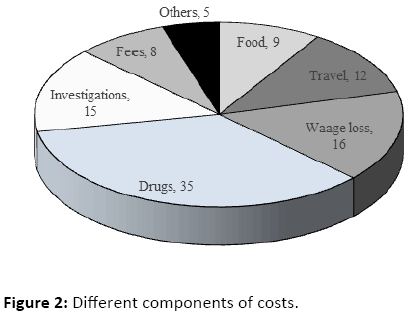
The overall average direct, indirect and total costs to patient with TB are given in Table 2. It was estimated that direct, indirect and total costs were averaging Rs.1642 (US$ 27.4), Rs. 1882 (US$ 31.4), and Rs.2466 (US$ 41.1) respectively. Overall direct and indirect costs were almost similar. Proportion of patients who incurred indirect costs was slightly higher than the proportion of patients who incurred direct costs both before and after diagnosis of TB. Figure 2 describes the different components of costs. Overall, patients spent more medical costs during shopping for diagnosis like medicines (35%) followed by investigations (15%), and fees (8%). A major proportion of non-medical cost incurred was due to wage lose (16%).
Cost for diagnosis
As this was a community survey to find out the TB cases (active case finding), around 86% of patients didn’t spent any costs for diagnosis and treatment (Table 2). Remaining patients incurred direct costs towards shopping for diagnosis before the survey which averaged mean Rs.1229; median Rs. 1000 as a direct costs. The average indirect costs was mean Rs. 573; median Rs.400 and total diagnosis cost was mean Rs. 1469; median Rs.1000 (Table 2). During diagnosis medical costs was higher than the non-medical costs (Rs.994 vs Rs. 331). Overall 45% of TB cases in this community get detected through active case finding; as they didn’t take any action for their symptoms. Remaining 46% approached government health facilities and 9% approached local healers (Table 3). The patient’s perception about the health facility access was also measured. It was found that majority (40%) found difficult to reach health facilities and 31% felt lack of money to approach health facility for diagnosis.
Costs for treatment
During the treatment none of the patient incurred any direct medical costs. The average direct non-medical cost was incurred for only 11% of patients and it was mean Rs.579 (US$ 9.65). Indirect costs was incurred for only 5% of patients, it was estimated to be mean Rs.1718 (US$ 28.6). Total treatment costs were also incurred for only 11% and it was mean Rs.1335 (US$ 22.25). It was observed that indirect treatment costs were higher than the direct costs (Rs.579 vs Rs.1718).
Those patients who didn’t spend any costs during treatment reported that majority (61%) of patients have taken treatment under the community DOT providers; 65% of patients DOT providers were living in the same village; 46% perceived that DOT is convenient to them; and 50% reported that they are satisfied with their DOT providers. However, 34% of patients returned from DOT centre more than once without medicine due to non-availability of DOT providers.
Catastrophic expenditure
In our sample, majority getting treatment free of costs and those who incurred costs, they faced catastrophic TB care expenditure amounted to 10%, which is the proportion of various costs in relation to annual family income (Figure 3).
The intensity of catastrophic health payments are shown on Figure 4. Results have shown that among 33 patients, six households reported the share of OOP payments were much exceeding their income (Figure 4).
Discussion
This study demonstrates the economic burden in terms of direct, indirect costs and total costs for both diagnosis and treatment of TB among Saharia tribe, a PVTG living in central India. Because of the profound connection between poverty and TB, our study confirms that TB patients are from vulnerable groups, having poor living conditions, depending on primitive agriculture, low cost closed economy based on low level of technology, working as a daily wage labourer and not having regular incomes before their disease. Average incomes are substantially lower due to the informal economy and there is a higher prevalence of impoverished employees working in the informal sector. It is very clear that majority of TB patients didn’t incur any costs due to active case finding. Very small proportion of patients incurred OOP payments due to shopping for diagnosis and non-medical costs during treatment was considerably high. Since Saharia’s are already economically poor and socially vulnerable becoming poor, many more are being trapped further into poorer due to the various costs of TB diagnosis and treatment. There is an urgent need; the Government of India should consider alternative health financing mechanisms that offer financial risk protection to the PVTGs in general and Saharia’s in particular.
RNTCP in India is the largest national TB control programme in the world and also financing to improve outcomes in tribal areas. It has addressed many challenges and special provisions were given in tribal areas for reducing financial burden to the TB patients throughout the course of treatment. Provisions for covering travel costs for patients and one attendant during treatment and follow-up are in place which aggregately amounts to Rs.250 (US$ 4.2) on completion of treatment. Volunteers are encouraged for sputum collection and transportation and provided Rs.100 to Rs.200 (US$ 1.7 to 3.3) per month per volunteer based on number of visits to designated microscopy centre (DMC) to hand over collected sputum. An amount of Rs.100 (US$ 1.7) per month if there is a minimum of one visit to the health center per week with collected samples [24]. There is a need to ensure the implementation of these schemes, and its functions and impact in these areas. Since the Saharia’s poor have less income, higher proportion of their expenditure goes towards food than TB treatment.
There was evidence from India that direct OOP payments could push 2.2% of all healthcare users and one-fourth of all hospitalized patients, into poverty in a year [25]. According to the national sample survey organization (NSSO) data 55th Round, households spend about 5%-6% of their total consumption expenditure on health [26]. As per RNTCP the case findings are passive, chest symptomatic expected to go to hospital on their own. Findings from the current series, patients are diagnosed through active case finding, majority (85%) did not incurred any costs. On the other hand, it could also mean that households do not seek care if they cannot afford it or due to non-availability of services. This emphasizes the earlier point that it is also important to explore the extent to which households do not use services because of inability to pay. It was reported that availability of services proved to be positively correlated with catastrophic spending in low and middle income countries but not in high income countries [27,28]. In many other European countries health insurance coverage is very comprehensive and OOP payments are either absent or do not differ across provider alternatives [29]. In low and middle income countries, supply constraints limit the use of services, so countries with greater supply show higher levels of use and more financial catastrophe. Increasing the availability of services in poor countries is important for improving health.
It was also observed from this study that small proportion of patients’ need to spend costs when they go for DOT in health facility based DOT centre or non-community based DOT provider. Also they need to spend for follow-up examinations and these costs are seem to be very high i.e. 10% of annual family income. Our study finding corroborate with the study done in Malawi and Kenya which reported that patient and household costs of TB diagnosis are prohibitively high where services are provided free of charge [22,30,31].
In tribal areas mostly travel facilities are poor and health centres are not always easily accessible due to this. A sick person may have to travel 25 km to reach the nearest PHC and patients may have to spend more for travel to attend these centres. The main occupation is agriculture which is mostly daily wages. Daily wage labourer going to faraway health centre may result in work absenteeism and loss of income. These costs made him/her to borrow money for treatment or manage family expenditure. This catastrophic expenditure forced them to very deprived position. OOP costs for public and private health-care services may stand at the beginning of a spiral into poverty for many families and exacerbate the poverty of the already poor. This situation has been termed as ‘medical poverty trap’ [32-34]. The loss of productive labour and frequently unaffordable expense of seeking treatment can thrust TB patients and their families deeper into poverty. When aggregated to the national level, the cost of TB to economic development and poverty reduction is tremendous [35]. However the encouraging finding is that due to active case finding many poor TB patients did not incurred any costs. Thus, TB control programme should consider active case finding strategy that provides financial risk protection to these kinds of vulnerable segments of population. So that the contribution of TB control contributes to alleviation of poverty by reducing the economic burden that the disease inflicts on the poor.
Government of India had invested a huge budget of US$ 252 million for the year of 2014 alone for National Tuberculosis Control Programme. The DOTS strategy was based on global scientific and operational guidelines and evidence, and that evidence has continued to evolve with time. As new evidences became available, the TB control programme has made necessary changes in its policies and programme management practices. In addition, with the changing global scenario, RNTCP is incorporating newer and more comprehensive approaches to TB control. To generate the evidence needed to guide policy makers and programme managers, the programme implemented measures to encourage operational research. Efforts of RNTCP to promote operational research yielded success and most of the studies are linked to the main priorities of TB control. The programme requires more knowledge and evidence of the effectiveness of interventions to optimize policies, improve service quality, and increase operational efficiency. The current study provided evidence on different dimension to improve TB and economic outcomes among poor people living in poor countries.
The RNTCP has continuously been innovative and progressive in addressing issues related to TB control in the country. The programme is decentralized and diagnosis and treatment is provided free of costs to all patients. Despite all this patients suffering from TB incurred out of pocket expenditure for travel, stay and food while shopping for diagnosis and treatment. When people have to pay fees if they go to private or traditional healers or co-payments for health care, the amount can be so high in relation to income that it results in ‘Financial Catastrophe’ for the individual or the household. Such high expenditures can mean that people have to cut down on necessities such as food and clothing, or are unable to pay for their children's education. It was estimated that every year, approximately 44 million households, or more than 150 million individuals, throughout the world face catastrophic expenditure, and about 25 million households or more than 100 million individuals are pushed into poverty by the need to pay for services [36]. Moreover, the impact of these OOP payments for health care goes beyond catastrophic spending alone. Many people may decide not to use services, simply because they cannot afford either the direct costs for consultations, medicines and laboratory tests, or the indirect costs, such as transport and special food. This was confirmed through our study findings which highlighted that 45% didn’t take any action for their symptoms suggestive of TB. DOTS may be failing to reach the poor because of the barriers that obstruct accessing TB control services along the pathway to cure from onset of symptoms to achieving a cure. Such impediments may undermine progress towards achieving the regional targets for TB control. Strategies are thus needed to improve the accessibility of DOTS for the poor. These strategies will also begin to address inequity in the burden of TB and access to TB control.
Limitations of the study
This study captures only the patients making OOP payments for health services and didn’t include people who need services but cannot afford them. This could be a limitation of our analysis. Also the data on OOP payment collected for different recall periods using different questions introduce more memory bias. But it is undoubtedly important to continue to develop the database and the methods to strengthen knowledge about this important topic.
Conclusion
TB is a disease that disproportionately affects the poor. TB control program therefore need to ensure that the economically and socially disadvantaged groups do not face barriers that keep them from seeking treatment. It is a major challenge, not only for TB control, but also for overall health system to protect households from the risk of impoverishment resulting from health expenditure, and to ensure that the population receives health services when needed. Decision makers can use the information presented in this paper to better target financial risk protection strategies. Although decision makers in the health sector do not control many of the levers necessary to reduce income inequality and poverty directly, they can do so indirectly. But, Ministry of Health can actively advocate for complementary policies to reduce social inequalities and increased funding for health because they can improve health, reduce the chances of financial catastrophe, help poor households escape from poverty, and contribute to overall economic growth.
Acknowledgment
The authors thank Dr Neeru Singh, Director, NIRTH, Jabalpur, for her encouragement and support throughout the study. The authors acknowledge the District Tuberculosis Officer, the WHO/ RNTCP consultant, District Tribal Welfare authorities, Block Medical Officers, and peripheral field staff in the district for the cooperation and assistance. Authors thank Ms Preeti Tiwari, Ms Swati Chouhan, Mrs Priyashri Tiwari Pandey and Ms Sneha Patel for data entry and cleaning.
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, et al. (2007) Protecting households from catastrophic health spending. Health Affairs 26: 972-983.
- Nhlema B, Kemp J, Steenbergen G, Theobald S, Tang S, et al. (2003) A systematic analysis of TB and poverty. WHO: 1-4.
- Rajeswari R, Balasubramanian R, Muniyandi M, Geetharamani S, Thresa X, et al. (1999) Socio-economic impact of tuberculosis on patients and family in India. See comment in PubMed Commons below Int J Tuberc Lung Dis 3: 869-877.
- Croft RA, Croft RP (1998) Expenditure and loss of income incurred by tuberculosis patients before reaching effective treatment in Bangladesh. Int J Tuberc Lung Dis 2: 252-254.
- Jackson S, Sleigh AC, Wang GJ, Liu XL (2006) Poverty and the economic effects of TB in rural China. See comment in PubMed Commons below Int J Tuberc Lung Dis 10: 1104-1110.
- Zhang T, Tang S, Jun G, Whitehead M (2007) Persistent problems of access to appropriate, affordable TB services in rural China: experiences of different socio-economic groups. See comment in PubMed Commons below BMC Public Health 7: 19.
- Hossain S, Quaiyum MA, Zaman K, Banu S, Husain MA, et al. (2012) Socio economic position in TB prevalence and access to services: results from a population prevalence survey and a facility-based survey in Bangladesh. See comment in PubMed Commons below PLoS One 7: e44980.
- Burman WJ, Dalton CB, Cohn DL, Butler JR, Reves RR (1997) A cost-effectiveness analysis of directly observed therapy vsself administered therapy for treatment of tuberculosis. Chest 112:63-70.
- Dholakia R (1997) The potential economic benefits of DOTS against TB in India. Global TB Programme of WHO.
- Floyd K, Wilkinson D, Gilks C (1997) Comparison of cost effectiveness of directly observed treatment (DOT) and conventionally delivered treatment for tuberculosis: experience from rural South Africa. See comment in PubMed Commons below BMJ 315: 1407-1411.
- Sawert H, Kongsin S, Payanandana V, Akarasewi P, Nunn PP, et al. (1997) Costs and benefits of improving tuberculosis control: the case of Thailand. See comment in PubMed Commons below SocSci Med 44: 1805-1816.
- Wilkinson D, Floyd K, Gilks CF (1997) Costs and cost-effectiveness of alternative tuberculosis management strategies in South Africa: Implications for policy. S Afr Med J 87: 451-455.
- Khatri GR, Frieden TR (2000) The status and prospects of tuberculosis control in India. See comment in PubMed Commons below Int J Tuberc Lung Dis 4: 193-200.
- Central TB Division. (2014) TB India 2014: RNTCP Status Report. New Delhi. Directorate of Health Services, Ministry of Health and Family Welfare.
- Chakma T, Vinay RP, Pall S, Kaushal LS, Manjula D,et al. (1996) Survey of pulmonary tuberculosis in a primitive tribe of Madhya Pradesh. Ind J Tub 43: 85-89.
- Rao VG, Gopi PG, Bhat J, SelvakumarN, Yadav R, et al. (2010) Pulmonary tuberculosis: a public health problem amongst Saharia, a primitive tribe of Madhya Pradesh, central India. Int J Infect Dis 14: e713-e716.
- The tool to estimate patients costs. USAID. The Tuberculosis Coalition for Technical Assistance.
- Russell S1 (2004) The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. See comment in PubMed Commons below Am J Trop Med Hyg 71: 147-155.
- Pradhan M, Prescott N (2002) Social risk management options for medical care in Indonesia. See comment in PubMed Commons below Health Econ 11: 431-446.
- Xu K, Evans DB, Kadama P, Nabyonga J, Ogwal PO, et al. (2006) Understanding the impact of eliminating user fees: utilization and catastrophic health expenditures in Uganda. See comment in PubMed Commons below SocSci Med 62: 866-876.
- O?Donnell O, Doorslaer EV, Wagstaff A, Lindelow M (2008) Analyzing health equity using household survey data: A guide to techniques and their implementation. World Bank Institute.
- Chuma J, Maina T (2012) Catastrophic health care spending and impoverishment in Kenya. See comment in PubMed Commons below BMC Health Serv Res 12: 413.
- Saksena P, Hsu J2, Evans DB2 (2014) Financial risk protection and universal health coverage: evidence and measurement challenges. See comment in PubMed Commons below PLoS Med 11: e1001701.
- Gupta SN, Gupta N, Gupta S (2013) Surveillance data analysis of Revised National Tuberculosis Control Program of Kangra, Himachal Pradesh. J Family Med Prim Care 2: 250-255.
- Peters DH, Yazbeck AS, Sharma RR, Ramana GNV, Pritchett LH, etal. (2002) Better health systems for India?s poor: Findings, analysis and options. Human Development Network (Health, nutrition, and population series): 1-376.
- National Sample Survey Organization (2001) Level and pattern of consumer expenditure, 1999?2000. Ministry of Statistics and Programme Implementation, Government of India.
- Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, et al. (2003) Household catastrophic health expenditure: a multicountry analysis. See comment in PubMed Commons below Lancet 362: 111-117.
- Chuma J, Gilson L, Molyneux C (2007) Treatment-seeking behaviour, cost burdens and coping strategies among rural and urban households in Coastal Kenya: an equity analysis. Trop Med Int Health 12:673-686.
- Varkevisser M, van der Geest SA, Schut FT (2010). Assessing hospital competition when prices don?t matter to patients: the use of time-elasticities.Int J Health Care Finance Econ 10: 43-60.
- Kemp JR, Mann G, Simwaka BN, Salaniponi FM, Squire SB (2007) Can Malawi's poor afford free tuberculosis services? Patient and household costs associated with a tuberculosis diagnosis in Lilongwe. Bull World Health Organ 85:580-585.
- Barter DM, Agboola SO, Murray MB, Bärnighausen T (2012) Tuberculosis and poverty: the contribution of patient costs in sub-Saharan Africa--a systematic review. See comment in PubMed Commons below BMC Public Health 12: 980.
- Whitehead M, Dahlgren G, Gilson L (2001) Developing the policy response to inequities in Health: a global perspective: Challenging inequities in health care: from ethics to action. New York, Oxford University Press: 309-322.
- Whitehead M, Dahlgren G (2006). Levelling up (part 1): a discussion paper on concepts and principles for tackling social inequities in health. WHO Regional Office for Europe.
- Iyer A (2005) Ill and impoverished: The medical poverty trap. InfoChange News & Features.
- World Health Organization (2004) Reaching the poor: challenges for the TB programmes in the Western Pacific Region. World Health Organization: Regional Office for the Western Pacific.
- World Health Organization (2005) Designing health finance systems to reduce catastrophic health expenditure. World Health Organization (WHO/EIP/HSF/PB/05.02).
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences