Disseminated Histoplasmosis with Breast Abscess in a Female with AIDS: Report of a Case and Review of the Literature
Marcelo Corti*, Fernando Messina F, Gabriela Santiso, Elena Maiolo, Mario Valerga and Ricardo Negroni
DOI10.21767/2471-8521.100017
1HIV/AIDS Division, Infectious Diseases F. J. Muniz Hospital, Buenos, Aires, Argentina
2Medicine Department, Infectious Diseases Orientation, University of Buenos Aires, School of Medicine, Argentina
3Mycology Unit, Infectious Diseases F. J. Muñiz Hospital, Buenos Aires, Argentina
- *Corresponding Author:
- Marcelo Corti
Infectious Diseases F. J. Muniz Hospital
Puan 381, 2nd floor
Postal Code C1406, Buenos Aires
Argentina
Tel: +54-11-44323762
E-mail: marcelocorti@fibertel.com.ar
Received date: July 25, 2016; Accepted date: August 26, 2016; Published date: September 06, 2016
Citation: Corti M, Messina FF, Santiso G, Maiolo E, Valerga M, et al. Disseminated histoplasmosis with breast abscess in a female with AIDS: Report of a case and review of the literature. Med Mycol Open Access 2016, 2:17. doi: 10.21767/2471-8521.100017.
Copyright: © 2016 Corti M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Histoplasmosis is a systemic mycosis, endemic in areas of subtropical and tropical climate. It is prevalent in North, Central and South America as well as in wide areas of Africa and Asia. Histoplasma capsulatum var. capsulatum is a dimorphic fungus that can cause a disseminated and severe disease in patients with impairment of cell-mediated immunity [1]. Disseminated histoplasmosis is a frequent opportunistic infection in AIDS patients in Argentina, with an incidence around 4% of the patients who required admission to the hospitals [2,3].
Herein, we present a case of a female with diagnosis of disseminated histoplasmosis with a breast gland abscess in a patient with AIDS.
Case Report
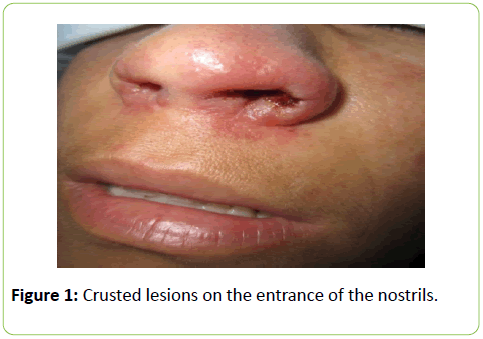
A 32 year-old female, HIV seropositive since 2002, with multiple withdrawal of highly active antiretroviral therapy (HAART) and a previous diagnosis of AIDS because she had diagnosis of disseminated histoplasmosis two years before. She was admitted to our Department of HIV/AIDS related illnesses with a history of fever, weight loss and epistaxis of 15 days duration. Physical examination revealed a temperature of 38°C, cachectic status, cutaneous papules and multiple crusted lesions, adherent, on the entrance of the nostrils (Figure 1). Breast examination showed asymmetric gynecomastia with abnormal growth of the left breast with marked left nipple retraction and a palpable mass of 3 x 3 cm in her left breast (Figure 2). The nodule was hard, mobile and painful and located on the left breast upper outer quadrant. A spontaneous purulent secretion by the nipple was seen. Routine laboratory.
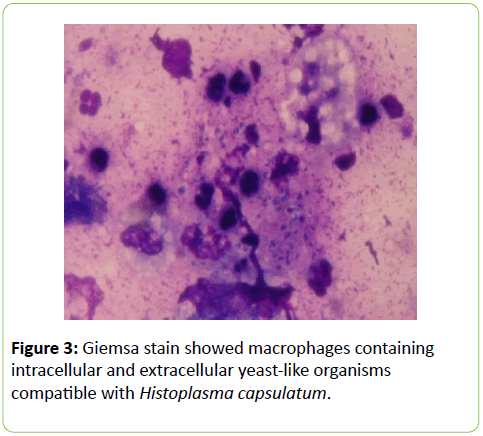
Investigation was performed, which showed hematocrit 32%, glycemia 92% mg, renal and liver function were normal. Hemocultures by lisis-centrifugation were negative. The CD4 Tcell count was of 84 cells/μl (5%). Chest X-ray was normal; abdominal ultrasound demonstrated a heterogeneous liver enlargement compatible with esteatosis and homogeneous splenomegaly. Breast ultrasonography examination with high frequency transducer was performed and revealed hypoechoic retroareolar lesion of 2 x 1,5 cm. Direct examination of purulent breast nipple secretion obtained with Pasteur pipette and stained with Giemsa showed macrophages containing intracellular and extracellular spherical to ovoid yeast-like organisms surrounded by a small light halo compatible with Histoplasma capsulatum (Figure 3). Also, scarification of skin lesion showed intracellular yeasts compatible with Histoplasma capsulatum.
Serologic test were negative, using immunodiffusion and double diffusion method.
Based on the microbiological findings, diagnosis of disseminated histoplasmosis was made; the patient was initially treated with 0.8 mg/kg/day of amphotericin B up to reach a total accumulated dose of 600 mg. Afterwards, he received 400 mg/day of oral itraconazole with clinical improvement and laboratory normalization. Treatment with amphotericin B followed by itraconazole resulted in complete remission of lesions.
Discussion
Histoplasmosis is the third potentially fatal opportunistic mycosis in patients with AIDS. Although disseminated criptococosis with CNS involvement, pneumocystosis and oropharyngeal candidiasis are present in patients with AIDS, in endemic areas, disseminated histoplasmosis is the most frequent mycosis in this population [4]. Disseminated disease is the most severe clinical form of histoplasmosis and is more likely to occur in immunocompromised individuals, especially those with advanced HIV/AIDS disease. Acute disseminated cases derive from the reactivation of latent foci of infection and are more severe in patients with AIDS than in those with other immunodeficiencies [5]. Disseminated histoplasmosis in AIDS patients is characterized by prolonger fever, weight loss, respiratory symptoms, pancytopenia, hepatosplenomegaly and mucocutaneous lesions.
Granulomatous mastitis secondary to Histoplasma capsulatum is a very infrequently reported entity; generally the patient presents with a history of a gradually increasing unilateral breast mass, as we could see in our case [6]. Also, physical examination may reveal skin retraction and signs of inflammation on the overlying skin, as in our patient.
Salfelder et al. [7] report 4 cases of granulomatous mastitis presenting as pseudotumors of the breast. Two of them were due Histoplasma capsulatum.
The most common mammographic finding is an asymmetrical density with a thickening of overlying skin. This aspect of the lesion may be clinically and radiographically difficult to distinguish from breast cancer [8].
Microscopic observation of characteristic yeast inside the cytoplasm is considered useful for the diagnosis, whenever observed by an experienced professional. In our case the material obtained from breast abscess was very little to be cultured.
The main differential diagnosis of granulomatous mastitis secondary to H. capsulatum includes other fungal infections, Mycobacterium tuberculosis, sarcoidosis, and idiopathic granulomatous mastitis [6].
Treatment of H. capsulatum breast abscess may include the complete excision followed by initial treatment with amphotericin B and oral itraconazole. Secondary prophylaxis with itraconazole is necessary in AIDS patients up to immune reconstitution associated with highly active antiretroviral therapy (HAART).
Conclusion
In conclusion, histoplasmosis should be considered in the differential diagnosis of the breast compromise as mastitis or abcesses in AIDS patients, especially when it is associated with prolonged febrile illness, weight loss and mucocutaneous lesions.
References
- Cohen PR, Groosman ME, Silvers DN (1991) Disseminated histoplasmosis and human immunodeficiency virus infection. Int J Dermatol 30: 614-622.
- Corti ME, Cendoya C, Soto I, Esquivel P, Trione N, et al. (2000) Disseminated histoplasmosis and AIDS: clinical aspects and diagnostic methods for early detection. AIDS Patient Care STDs 14: 149-154.
- Gutierrez ME, Canton A, Sosa N, Puga E, Talavera L (2005) Disseminated histoplasmosis in patients with AIDS in Panama: a review of 104 cases. Clin Infect Dis 40: 1199-1202.
- Corti M,Negroni R, Esquivel P, Villafane MF (2004) Histoplasmosisdiseminada en pacientes con sida: análisisepidemiológico, clínico, microbiológico e inmunológico de 26 pacientes. EnfEmerg 6: 8-15.
- Solari R, Corti M, Cangelosi D, Escudero M, Negroni R, et al. (2007) Disseminated histoplasmosis with lesions restricted to the larynx in a patient with AIDS. Report of a case and review of the literature. Rev IberoamMicol 24: 164-166.
- Payne S, Kim S, Das K, Mirani N (2006) A 36-Year-Old Woman With a Unilateral Breast Mass. Arch Pathol Lab Med 130: e1-e2.
- Salferder K, Schwarz J (1975) Mycotic "pseudotumors" of the breast. Report of four cases. Arch Surg 110: 751-754.
- Osborne BM (1989) Granulomatous mastitis caused by histoplasma and mimicking inflammatory breast carcinoma. Hum Path 20: 47–52.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences