Epidemiology and Clinical Characteristics of Cryptococcal Meningitis in China (1981-2013): A Review of the Literature
Zhu Li, Yongquan Liu, Hong Cao, Shenghe Huang and Min Long
DOI10.21767/2471-8203.100022
Zhu Li1, Yongquan Liu2ÃÆïÃâüÃâà âHong Cao2ÃÆïÃâüÃâà âShenghe Huang3 and Min Long*2
1Laboratory P3, Guangdong Provincial Key Laboratory of Tropical Disease Research, School of Public Health, Southern Medical University, Guangzhou 510515, China
2Department of Microbiology, Guangdong Provincial Key Laboratory of Tropical Disease Research, School of Public Health, Southern Medical University, Guangzhou 510515, China
3Department of Pediatrics, The Saban Research Institute, Children’s Hospital Los Angeles, Keck School of Medicine, University of Southern California, Los Angeles, CA 90027, California
- *Corresponding Author:
- Min Long
Department of Medical Microbiology
Southern Medical University
Guangzhou 510515, China
Tel: 86-13544304831
Fax: 86-20-61648324
E-mail: longmin@smu.edu.com
Received Date: December 30, 2016; Accepted Date: January 31, 2017; Published Date: February 10, 2017
Citation: Li Z, Liu Y, Cao H, Huang S, Long M (2017) Epidemiology and Clinical Characteristics of Cryptococcal Meningitis in China (1981-2013): A Review of the Literature. Med Mycol Open Access 3:1. doi: 10.21767/2471-8521.100022.
Copyright: © 2017 Li Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
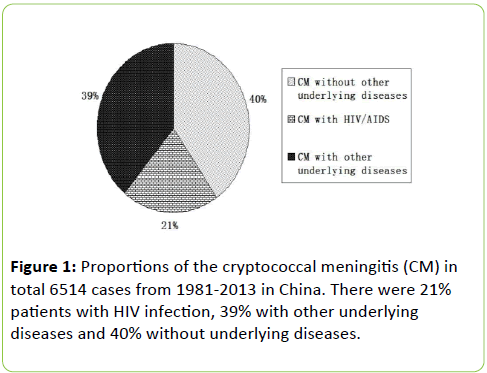
Most of patients with cryptococcal meningitis in China were not HIV victims. Profile of the diseases in patients with non-HIV infection was poorly understood. We summarized the epidemiology and clinical characteristics of cryptococcal meningitis in China. A comprehensive analysis of the reported cases of cryptococcal meningitis in China was conducted, covering publications from 1981 to 2013 from CNKI database. Among the 306 reports and 6514 cases about cryptococcal meningitis, there were 21% patients with HIV infection, 39% with other underlying diseases and 40% without underlying diseases. Main underlying diseases in non-HIV/AIDS patients were tuberculosis (10.46%), liver disease (9.83%), systemic lupus erythematosus (7.00%), diabetes (5.26%), kidney disease (3.16%), lung disease (2.97%), and cancer (2.01%). About 60.8% cases were reported in males. From 1981-2013 total patients of cryptococcal meningitis were increased. Patients who received treatment of amphotericin B (AmB) with 5-flucytosine, AmB with Fluconazole, and the combination of AmB+5-FU+FCZ were 495, 411, 266 persons (total 1501 cases) and got a total efficiency of 70.1%, 70.8%, and 74.8% respectively. The survival rate of cryptococcal meningitis patients without HIV infection is higher than those with HIV infection (p<0.05). The result shows that most patients of cryptococcal meningitis have underlying diseases and there is a connection between cryptococcal meningitis and immunodeficiency in China.
Summary
Most of patients with cryptococcal meningitis in China were not HIV victims. Profile of the diseases in patients with non-HIV infection was poorly understood. We summarized the epidemiology and clinical characteristics of cryptococcal meningitis in China. A comprehensive analysis of the reported cases of cryptococcal meningitis in China was conducted, covering publications from 1981 to 2013 from CNKI database. Among the 306 reports and 6514 cases about cryptococcal meningitis, there were 21% patients with HIV infection, 39% with other underlying diseases and 40% without underlying diseases. Main underlying diseases in non-HIV/AIDS patients were tuberculosis (10.46%), liver disease (9.83%), systemic lupus erythematosus (7.00%), diabetes (5.26%), kidney disease (3.16%), lung disease (2.97%), and cancer (2.01%). About 60.8% cases were reported in males. From 1981-2013 total patients of cryptococcal meningitis were increased. Patients who received treatment of amphotericin B (AmB) with 5-flucytosine, AmB with Fluconazole, and the combination of AmB+5-FU+FCZ were 495, 411, 266 persons (total 1501 cases) and got a total efficiency of 70.1%, 70.8%, and 74.8% respectively. The survival rate of cryptococcal meningitis patients without HIV infection is higher than those with HIV infection (p<0.05). The result shows that most patients of cryptococcal meningitis have underlying diseases and there is a connection between cryptococcal meningitis and immunodeficiency in China.
Keywords
Cryptococcus neoformans; Cryptococcal meningitits; HIV; Epidemiology
Introduction
Cryptococcus neoformans (C. neoformans) is the most important cause of invasive fungal disease. It is neurotropic and provokes the onset of cryptococcal meningitis. In HIV/AIDS patients with severe immunodeficiency, C. neoformans is a dangerous opportunistic infection [1]. Worldwide, C. neoformans and C. gattii infections cause approximately one million cases of cryptococcal meningitis per year among people with HIV/AIDS, resulting in nearly 625,000 deaths (Centers for Disease Control and Prevention, CDC, Atlanta, USA, https:// www.cdc.gov/). Cryptococcal meningitis also occurs in patients with non-HIV infection. In the absence of HIV, the disease occurs most commonly in people with decreased immunity, such as the patients with sarcoidosis and lymphoproliferative disorders, as well as patients undergoing immunosuppressive therapies, malignancy or organ transplantation [2]. However, it also occurs in immunocompetent people, though very rarely [3-4].
In Europe and the United Statesabout 80% of the cryptococcosis cases were associated with HIV/AIDS. But in China, recent reports revealed that the majority of patients with cryptococcosis were not HIV victims [5,6]. Cryptococcal meningitis is a life-threatening infection with noteworthy morbidity and mortality. This infection has been increasing steadily over the past years in China. It is unclear whether these patients have other underlying diseases except HIV/AIDS and they are mostly in immunodeficient or immunocompetent state.
Therefore, we carried out a descriptive study on the case reports from 1981 to 2013 to summarize the epidemiology and clinical characteristics of cryptococcal meningitis in China.
Method
A comprehensive analysis of reported cases of cryptococcal meningitis from China was conducted, covering publications from 1981 to 2013, using China Academic Journal Network Publishing Database (China National Knowledge Infrastructure, CNKI), Wanfang data, and the CBMdisk database (China Biology and Medicine data disc, Institute of Medical Information, Chinese Academy of Medical Sciences), by two separated authors. All cases were collected from above database with key words of cryptococcus and meningitis and case.
Case definition: Cryptococcal meningitis was defined as follows: Positive cerebrospinal fluid (CSF) India ink examination of C. neoformans or positive CSF cryptococcal antigen test or positive CSF cryptococcal culture. Some cases were confirmed through the pathology examination of brain tissue. Cryptococcal was found in the brain tissue taken by biopsy or operation.
Statistic analysis: SPSS 13.0 software was used for analyzing data. Statistical significance was set at alpha=0.05.
Results
Population distribution of Cryptococcal meningitis
In the total cases of Cryptococcal meningitis analyzed, 21% of the patients had HIV infection, 39% had other underlying diseases, while another 40% did not have any identifiable underlying diseases (Figure 1).
Incidence trend of Cryptococcal meningitis in China
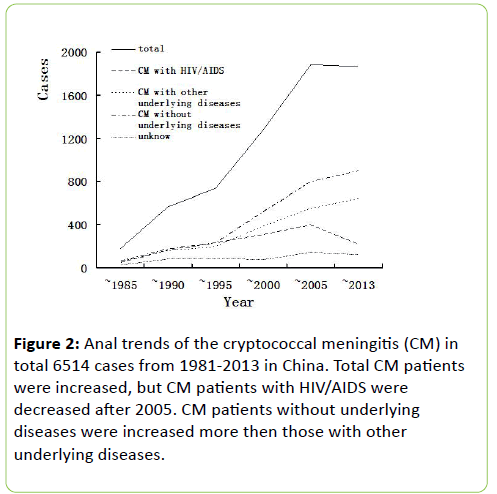
From anal trends of the cryptococcal meningitis in total 6514 cases (1981-2013), the result shows that total cases were increased rapidly, the patients of cryptococcal meningitis without underlying diseases were increased more than those with other underlying diseases, but the patients with HIV/AIDS were decreased after 2005 (Figure 2).
Sex ratio and occupation of Cryptococcal meningitis in China
A total of 6514 cases of cryptococcal meningitis were reported in 306 published articles, including 3961 male and 2375 female. There were more male patients (60.81%) than female ones (36.46%), which may be contributed by the differential interaction between C. neoformans and macrophages within different gender environments (Table 1). Macrophages from females phagocytose more C. neoformans [5]. Occupation of patients is farmer, worker, staff member, unemployed and student in turn (Table 1).
| Sex | Cases | % |
|---|---|---|
| Male | 3961 | 60.81% |
| Female | 2375 | 36.46% |
| Unknown | 178 | 2.73% |
| Total | 6514 | 100% |
| Occupation | ||
| Farmer | 405 | 46.88% |
| Worker | 130 | 15.05% |
| Staff member | 76 | 8.80% |
| Unemployed | 69 | 7.99% |
| Students | 54 | 6.25% |
| other | 130 | 15.05% |
| Total | 864 | 100% |
Table 1: Sex comparison and occupation of patients with cryptococcal meningitis in China, 1981-2013
Underlying disease of Cryptococcal meningitis in China
In the 60% patients with underlying diseases, the most common underlying disease is HIV/AIDS (40.66%), the second most one is tuberculosis (10.46%), other diseases included (in the order of decreasing frequency): liver disease (9.83%), systemic lupus erythematosus (7.00%), diabetes (5.26%), kidney disease (3.16%), lung disease (2.97%), cancer (2.01%) and so on (Table 2).
| Underlying diseases | Cases | % |
|---|---|---|
| HIV/AIDS | 1353 | 40.66% |
| Tuberculosis | 348 | 10.46% |
| Liver disease | 327 | 9.83% |
| SLE | 233 | 7.00% |
| Diabetes | 175 | 5.26% |
| Kidney disease | 105 | 3.16% |
| Lung disease | 99 | 2.97% |
| Cancer | 67 | 2.01% |
| Hormone usage | 55 | 1.65% |
| Antibiotic usage | 53 | 1.59% |
| Organ transplant | 38 | 1.14% |
| Leukemia | 31 | 0.93% |
| Anemia | 30 | 0.90% |
| Rheumatoid arthritis | 29 | 0.87% |
| Others | 385 | 11.57% |
| Total | 3328 | 100% |
Note: SLE: systemic lupus erythematous
Table 2: Distribution of the underlying diseases of patients with cryptococcal meningitis
Laboratory examination of Cryptococcal meningitis
Laboratory examination of crypotococcal meningitis usually included CD4 cell count, CSF (cerebrospinal fluid) pressure measurement, and CSF biochemical as well as other CSF conventional examinations. According to the detection of CD4 cell of 910 AIDS patients, 77.58% patients had CD4 cells levels under 200 cells/μl, including 46.68% less than 50 cells/μl, 23.19% between 50 and 100 cells/μl, and 5.71% between 100 and 200 cells/μl (Table 3). This result showed that the lower CD4 cells the AIDS patients was the more susceptible to opportunistic infections. However, in patients without HIV infection, the examination of CD4 cell level was not carried out, adding to the mystery whether the patients of cryptococcal meningitis with non-HIV infection were in immunodeficient state.
| CD4 counts (×106/L) | Cases | % |
|---|---|---|
| ÃÆïÃâüÃâà â50 | 443 | 48.68% |
| 50-100 | 211 | 23.19% |
| 100-200 | 52 | 5.71% |
| ÃÆïÃâüÃâà ¾200 | 15 | 1.65% |
| Reduce | 186 | 20.44% |
| Normal | 3 | 0.33% |
| Total | 910 | 100% |
Table 3: CD4 cell counts of patients of Cryptococcal Meningitis with HIV/AIDS
CSF pressure measurement, biochemical examination, and other conventional examinations help for the early diagnosis of cryptoccocal meningitis and help to improve its diagnostic rates. A total number of 4721 patients checked lumbar puncture pressure of CSF, and 4340 patients had high pressure (91.9%). Among 3441 patients taken lumbar puncture CSF white blood cell count, 3104 (90.2%) patients showed increased white blood cells. In 3807 patients taken lumbar puncture CSF protein test, 3231 (84.8%) patients showed increased protein amount. However, 3280 out of 4056 (80.8%) patients showed reduced glucose amount, and 3006 out of 3983 (75.5%) patients showed reduced chlorine amount (Table 4).
| CSF | Pressure | WBC | Protein | Glucose | Chlorine |
|---|---|---|---|---|---|
| Increase | 4340 | 3104 | 3231 | 43 | 60 |
| Normal | 381 | 248 | 563 | 733 | 917 |
| Reduce | 0 | 89 | 13 | 3280 | 3006 |
| Unknown | 1793 | 3073 | 2707 | 2458 | 2531 |
| Total | 6514 | 6514 | 6514 | 6514 | 6514 |
Note: CSF: cerebrospinal fluid
Table 4: CSF examination of patients with cryptococcal meningitis
Treatment protocols and prognosis of Cryptococcal meningitis
In total 6514 cases, 1605 cases shared the details of their treatment protocols and prognosis: 563 cured, 578 improved, 399 dead and 65 discharged, leading to a total effic iency of 71.9%. The number of patients who received treatment of amphotericin B (AmB) with 5-flucytosine (5-FU), AmB with Fluconazole (FCZ), and the combination of AmB+5-FU+FCZ were 495, 411, 266 persons and got a total efficiency of 70.1%, 70.8%, and 74.8% respectively. There is also single treatment by AmB only or FCZ only, each with 64.3% and 65.3% efficiency (Table 5). Other treatment protocols included usage of allicin, clotrimazol,s itraconazole, voriconazole, thymosin combined with AmB, FCZ,5-FC. By comparison, treatment with AmB+FCZ+5FC trigeminy is most effective.
| Treatment | Cases | Cure | Improvement | Death | Discharge | Effective% |
|---|---|---|---|---|---|---|
| AMB+5FC | 495 | 150 | 197 | 129 | 19 | 70.1 |
| AMB+FCZ | 411 | 142 | 149 | 95 | 25 | 70.8 |
| AMB+FCZ+5FC | 266 | 106 | 93 | 57 | 10 | 74.8 |
| AMB | 199 | 80 | 48 | 64 | 7 | 64.3 |
| FCZ | 130 | 50 | 35 | 42 | 3 | 65.3 |
| total | 1501 | 528 | 522 | 387 | 64 | 69.1 |
Note: AmB: amphotericin B, 5FC: 5-fluorocytosine, FCZ: fluconazole
Table 5: The comparison of outcome of patients treated with different protocols
Outcome of Cryptococcal meningitis in HIV/AIDS patients and non-HIV/AIDS patients
There were totally 5162 non-HIV/AIDS patients, with a cure rate of 24.41%, improvement rate of 25.80%, and mortality rate of 24.74%. As for the 1352 HIV/AIDS patients, the cure rate was 9.17%, improvement rate was 37.43%, and mortality rate was 31.07%. This showed that non-HIV/AIDS patients had a higher cure rate yet HIV/AIDS patients had a higher mortality (Table 6). In addition, the survival rate of 2592 non-HIV/AIDS patients was 66.99%, while the survival rate of 630 HIV/AIDS patients was 60%, showing that non-HIV/AIDS patients had higher survival rate than HIV/AIDS patients (p0.05) (Table 6).
| Outcome | non-HIV/AIDS | HIV/AIDS | ||
|---|---|---|---|---|
| cases | % | cases | % | |
| Cure | 1,260 | 24.41 | 124 | 9.17 |
| Improvement | 1,332 | 25.8 | 506 | 37.43 |
| Death | 1,277 | 24.74 | 420 | 31.07 |
| *Survival rate | 66.99 | 60 | ||
| Survival | 2592 | 66.99 | 630 | 60 |
| Death | 1277 | 33.01 | 420 | 40 |
*Pearson Chi-Square test, value=17.878,p<0.05.
Table 6: The comparison of outcome of cryptococcal meningitis cases with and without HIV/AIDS
Discussion
We found that in China, only 21% of the cryptococcal meningitis patients were with HIV infection. This result contradicts those reports saying that HIV/AIDS was associated with cryptococcosis in about 80% of the cases in Europe and the United States [6], and 69% of the cases in Africa [7]. However, such a result coincides with the documentations of cryptococcal meningitis in Australia, New Zealand, and India, where a relatively high percentage of the patients suffering from cryptococcosis were non-HIV infected [8]. Most of these patients in Australia and New Zealand were in immunocompromised state [9]. Cryptococcal meningitis in Viet Nam also occurs commonly in non-HIV/AIDS patients and most patients (81%) have no concomitant immunosuppressive disease, although CD4 lymphopenia was detected in some patients [2].
In China, most of the cryptococcal meningitis (60%) patients have underlying diseases, which increase the possibility that patients are in immunodeficient state. The most common underlying disease was HIV/AIDS, the second was tuberculosis, and liver diseases came in third, and other underlying diseases. During our investigation, we found that among the patients of cryptococcal meningitis with HIV/AIDS 69.87% had CD4 cell count less than 100 cells/μl, 46.68% had CD4 cell count less than 50 cells/μl, and 23.19% between 50 to 100 cells/μl. This shows that opportunistic C. neoformans infection of the central nerves system occurs mainly in severely immunocompromised HIV/AIDS patients. Tuberculosis and liver diseases were also very commonly seen in cryptococcal meningitis patients, probably due to the high prevalence of tuberculosis and hepatitis B in China [10,11]. This result is consistent with another report from China about cryptococcosis [12]. Though we did not test the CD4 cell number of patients without HIV infection, it was known that tuberculosis and hepatitis B occur in cell-immunity insufficient persons [13,14]. It was also known that other underlying diseases included systemic lupus erythematosus, diabetes, kidney diseases,lung disease, cancer, hormone usage, antibiotic usage, organ transplant, leukemia, anemia, rheumatoid arthritis and others, many of which were proved to be associated with immunosuppressive condition. Moreover, in Vietnam, 9 of 57 patients of cryptococcal meningitis in non-HIV infected population had CD4 counts of less than 400 cells/μl [2]. Therefore, we strongly believe that cryptococcal meningitis mainly occurs in immunodeficient people in China. But about 40% patients of cryptococcal meningitis were without any identifiable underlying diseases. The reasons should be further explored.
From anal trends of the cryptococcal meningitis in total 6514 cases (1981-2013), we found that total cases were increased rapidly, the patients of cryptococcal meningitis without underlying diseases were increased more than those with other underlying diseases, but the patients with HIV/AIDS were decreased after 2005. Maybe recently the highly active antiretroviral therapy (HAART) improved survival and significantly reduced the opportunistic infection incidence in HIV/AIDS patients.
Early symptoms of Cryptococcal meningitis are not specific. The onset of this disease was mostly chronic or subacute, so it was often misdiagnosed [15]. The clinical manifestations and changes of cerebrospinal fluid caused by cryptococcal meningitis are very similar to the tuberculous meningitis, so it is always misdiagnosed as tuberculous meningitis [16]. Clinicians should strengthen the understanding of cryptococcal meningitis by taking it into account when patients show symptoms of headache and meningeal irritation. Clinicians should also pay attention to check the existence of C. neoformans through CSF examination. To improve the positive rate, repeated examinations of the CSF for C. neoformans must be carried out [17]. However, this method is often limited when the number of the fungus is too few to be identified. Another commonly used method is the latex agglutination test of cryptococcal antigen (LACT) in serum or CSF, which is very specific, rapid, and accurate [18].
It was known that amphotericin B is the most common drug for the treatment of cryptococcal meningitis [19] and achieved in a total efficiency of 60–70% [20]. In our report, patients who received treatment of AmB with 5-FU, AmB with FCZ, and the combination of AmB+5-FU+FCZ were 495, 411, 266 persons and got a total efficiency of 70.1%, 70.8%, and 74.8% respectively. The combination of AmB with 5-FU and AmB with FCZ were often available and more effective for the treatment of cryptococcal meningitis in China. Treatment with AmB+FCZ+5FC trigeminy is most effective. As for the treatment of HIVassociated cryptococcal meningitis, it consists of three phases: induction, consolidation, and maintenance [21]. Although later relapse is unlikely to occur during successful ART (antiretroviral therapy), lifelong fluconazole is still recommended after the presence of cryptococcal meningitis [22,23].
In our study there were more male patients (60.81%) than female ones (36.46%). The male predominance maybe attributed to increased environmental exposure, hormonal influences, and/or genetic predisposition [3,5]. It was also showed that non-HIV/AIDS patients had a higher cure rate yet HIV/AIDS patients had a higher mortality. And non-HIV/AIDS patients had higher survival rate than HIV/AIDS patients (p<0.05)
Cryptococcal meningitis is a potentially fatal disease. In China, due to the lack of experience and the lack of mycology laboratories on the diagnosis of cryptococcal meningitis, many cases were misdiagnosed and missed the best treatment time. Known underlying diseases, such as AIDS, tuberculosis, liver diseases, SLE, diabetes, kidney diseases and so on, are often difficult to treat or always incurable. Therefore, the mortality of cryptococcal meningitis is high, cure rate is not very high and relapse occurs easily. To further raise the cure rate of cryptococcal meningitis, clinicians and relevant agencies should pay more attention to prophylaxis and prompt treatment for cryptococcal meningitis.
References
- Ssekitoleko R, Kamya MR, Reingold AL (2013) Primary prophylaxis for cryptococcal meningitis and impact on mortality in HIV: a systematic review and meta-analysis. Future Virol 8.
- Tran TC, Nguyen HM, Nguyen HP (2010) A prospective descriptive study of cryptococcal meningitis in HIV uninfected patients in Vietnam - high prevalence of Cryptococcus neoformans var grubii in the absence of underlying disease. BMC Infect Dis 10: 199.
- Chen J, Varma A, Diaz MR (2008) Cryptococcus neoformans strains and infection in apparently immunocompetent patients, China. Emerg Infect Dis 14: 755-762.
- Liao Y, Chen MÃÆïÃâüÃâà âHartmann T (2013) Epidemiology of opportunistic invasive fungal infections in China: review of literature. Chin Med J (Engl) 126: 361-368.
- McClelland EE, Hobbs LM, Rivera J (2013) The role of host gender in the pathogenesis of Cryptococcus neoformans infections. PLoS One 8: e63632.
- Wei Fang, Zhenzong Fa, Wanqing Liao (2015) Epidemiology of Cryptococcus and cryptococcosis in China. Fungal Genetics and Biology 78: 7-15
- Antinori S (2013) New Insights into HIV/AIDS-Associated Cryptococcosis. Isrn Aids 471363
- Anastasia P, Litvintseva, Ignazio Carbone (2011) Evidence that the human pathogenic fungus Cryptococcus neoformans var. grubii may have evolved in Africa. PLoS One 6: e19688.
- Jain N, Wickes BL, Keller SM (2005) Molecular epidemiology of clinical Cryptococcus neoformans strains from India. J Clin Microbiol 43: 5733-5742.
- Chen S, Sorrell T, Nimmo G (2000) Epidemiology and host- and variety-dependent characteristics of infection due to Cryptococcus neoformans in Australia and New Zealand. Australasian Cryptococcal Study Group. Clin Infect Dis 31: 499-508.
- Huang ML, Xu XT, Shen J, Qiao YQ, Dai ZH, et al. (2014) Prevalence and factors related to hepatitis B and C infection in inflammatory bowel disease patients in China: A retrospective study. J Crohns Colitis 8: 282-287.
- Wang L, Zhang H, Ruan Y (2014) Tuberculosis prevalence in China, 1990-2010; a longitudinal analysis of national survey data. Lancet 383: 2057-2064.
- Yuchong C, Fubin C, Jianghan C (2012) Cryptococcosis in China (1985-2010): review of cases from Chinese database. Mycopathologia 173: 329-335.
- Ichiki Y, He XS, Shimoda S (2005) T cell immunity in hepatitis B and hepatitis C virus infection: implications for autoimmunity. Autoimmun Rev 4: 82-95.
- Prezzemolo T, Guggino G, La Manna MP, Di Liberto D, Dieli F, et al. (2014) Functional Signatures of Human CD4 and CD8 T Cell Responses to Mycobacterium tuberculosis. Front Immunol 5: 180.
- Xie D, Cao H, Yu H (1999) Differential diagnosis in patients with tuberculous meningitis and cryptococcal meningitis. Zhonghua Jie He He Hu Xi Za Zhi 22: 731-733.
- Zhang B, Lv K, Bao J, Lu C, Lu Z (2013) Clinical and laboratory factors in the differential diagnosis of tuberculous and cryptococcal meningitis in adult HIV-negative patients. Intern Med 52: 1573-1578.
- Cohen DB, Zijlstra EE, Mukaka M (2010) Diagnosis of cryptococcal and tuberculousmeningitis in a resource-limited African setting. Trop Med Int Health 15: 910-917.
- Dominic RS, Prashanth H, Shenoy S, Baliga S (2009) Diagnostic value of latex agglutination in cryptococcal meningitis. J Lab Physicians 1: 67-68.
- Perfect JR, Dismukes WE, Dromer F (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis 50: 291-322.
- Bennett JE, Dismukes WE, Duma RJ (1979) A comparison of amphotericin B alone and combined with flucytosine in the treatment of cryptoccal meningitis. N Engl J Med 301: 126-131.
- Sloan DJ, Parris V (2014) Cryptococcal meningitis: epidemiology and therapeutic options. Clin Epidemiol 6: 169-182.
- Seddon J, Mangeya N, Miller RF (2009) Recurrence of cryptococcal meningitis in HIV-infected patients following immune reconstitution. Int J STD AIDS 20: 274-275.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences