Subcutaneous Abscess as a Single Manifestation of Candidiasis
Marcelo Corti,Maria F Villafane,Fernando Messina and Ricardo Negroni
DOI10.21767/2471-8521.100006
Marcelo Corti1,2*, Mar?a F Villafa?e1,2, Fernando Messina3 and Ricardo Negroni3
1HIV/AIDS Division and Mycology Unit, Infectious Diseases F. J. Mu?iz Hospital, Buenos Aires
2Medicine Department, Infectious Diseases Orientation, University of Buenos Aires, School of Medicine, Argentina
3Mycology Unit, Infectious Diseases F. J. Mu?iz Hospital, Buenos Aires
- *Corresponding Author:
- Marcelo Corti
Infectious Diseases F. J. Mu?iz Hospital
Puán 381, 2nd floor
Postal Code C1406
Tel: +54-11-44323762
E-mail: marcelocorti@fibertel.com.ar
Received date: August 17, 2015; Accepted date: November 25, 2015; Published date:December 05, 2015
Citation: Corti M, Villafañe MF, Messina F, et al. Subcutaneous Abscess as a Single Manifestation of Candidiasis. Med Mycol Open Access. 2015, 1:6. doi: 10.21767/2471-8521.100006
Copyright: © 2015 Corti M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Candida is yeast responsible for the majority of the systemic invasive fungal infections in humans. The incidence of systemic Candida infections has increased, probably due to a rising number of patients with comorbidities and risk factors for invasive candidiasis. Candidemia is a life-threatening infection with high morbidity and mortality especially in individuals at greatest risk of fungal infection, such as patients receiving cancer chemotherapy, immunosuppressive therapy, prolonged antibiotic therapy, neutropenia, recent abdominal surgery, hematological malignancies, central venous catheter, receipt of corticosteroids, parenteral nutrition, etc. In patients infected with the human immunodeficiency virus (HIV) the predominant clinical forms of candidiasis include the mucosal involvement as oral candidiasis, oesophageal candidiasis, Candida vaginitis and Candida balinitis [1]. Although subcutaneous abscess due to Candida species is frequent in non-neutropenic patients after transient candidemia, it is a rare complication in immunocomprimised patients due to HIV/AIDS disease. The few cases reported in the medical literature occur as a complication of bacterial cellulitis, iatrogenic injury, trauma or intravenous drug abuse [2]. We present the clinical history of an HIV patient who developed a subcutaneous abscess due to Candida albicans without fungemia or other focal manifestation of this mycosis.
Introduction
Candida is yeast responsible for the majority of the systemic invasive fungal infections in humans. The incidence of systemic Candida infections has increased, probably due to a rising number of patients with comorbidities and risk factors for invasive candidiasis. Candidemia is a life-threatening infection with high morbidity and mortality especially in individuals at greatest risk of fungal infection, such as patients receiving cancer chemotherapy, immunosuppressive therapy, prolonged antibiotic therapy, neutropenia, recent abdominal surgery, hematological malignancies, central venous catheter, receipt of corticosteroids, parenteral nutrition, etc. In patients infected with the human immunodeficiency virus (HIV) the predominant clinical forms of candidiasis include the mucosal involvement as oral candidiasis, oesophageal candidiasis, Candida vaginitis and Candida balinitis [1]. Although subcutaneous abscess due to Candida species is frequent in non-neutropenic patients after transient candidemia, it is a rare complication in immunocomprimised patients due to HIV/AIDS disease. The few cases reported in the medical literature occur as a complication of bacterial cellulitis, iatrogenic injury, trauma or intravenous drug abuse [2]. We present the clinical history of an HIV patient who developed a subcutaneous abscess due to Candida albicans without fungemia or other focal manifestation of this mycosis.
Case report
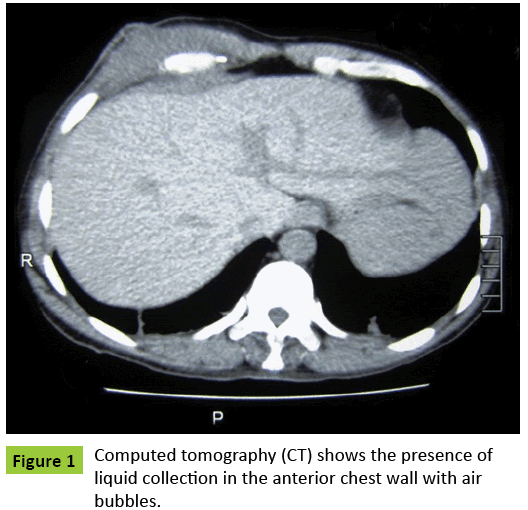
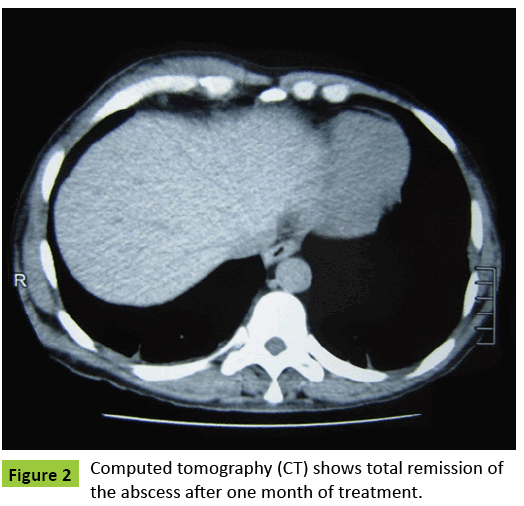
A 42-year-old HIV-seropositive man was admitted to the HIV/AIDS department of our hospital with a painful subcutaneous abscess on the right chest wall. He had diagnosis of AIDS because he had suffered a cerebral toxoplasmosis one year ago. After that, he was started on highly active antiretroviral therapy (HAART) including Zidovudine, Lamivudine and Efavirenz. Laboratory findings were normal, including liver and renal function tests; serological status for HCV virus was negative; the last CD4 T cell count was 145 cell/ μl and the plasma viral load was undetectable. A subcutaneous ultrasound revealed a heterogeneous image of 33.4 mm × 10 mm, with irregular contours with echogenic stippling and hypo echoic area in intimate contact with the muscular plane. A computed tomography (CT) confirmed the presence of a liquid collection in relation to the anterior chest wall with air bubbles (Figure 1). A surgical drainage was performed. A purulent material was obtained and Candida albicans was isolated in fungal cultures. The susceptibility of Candida albicans by MIC microdilution to voriconazole was 0.032 μg/ml; to amphotericin B: 0.064 μg/ml; to fluconazole: 1.0 μg/ml, to itraconazole: 0.50 μg/ml and to caspofungin was 0.032 μg/ml. Blood cultures were negative for bacteria, mycobacteria and fungus. An echocardiography showed no pathological alterations and the abdominal ultrasound revealed homogeneous hepatomegaly and splenomegaly. An ocular fundoscopy was normal. The patient received fluconazole 400 mg daily with a total remission of the abscess after one month of treatment (Figure 2).
Discussion
Subcutaneous abscess due to Candida albicans is a rare and infrequent complication in absence of other focal visceral disease, except in non-neutropenic patients who are intravenous addict to "brown" heroin and develop transient candidemia [3]. Nodular cutaneous lesions or subcutaneous abscess occurs in 10% of cases in disseminated candidiasis of neutropenic patients [4]. In a review of 375 fungal isolations, Candida albicans was recovered from pus in only one patient [5]. Risks factors for Candida infection includes HIV infection, as in our patient, in which mucosal site colonized with Candida species is a frequent clinical complication [6]. The adherence capacity and the ability to form biofilms may be an important fungal virulence factor to all Candida species [7,8]. Subcutaneous abscess due to Candida albicans has been described only in patients with other underlying diseases or with lesions of the skin. Candida infection of subcutaneous tissue may result from trauma, inoculation injury or hematogenous spread [9]. The site of abscess in our case was the lower thoracic wall and no break of the skin integrity was present. Although blood cultures, bi-dimensional echocardiography and ocular fundoscopy were negative for Candida and no other focus of infection was found, we cannot exclude hematogenous spread that can explain the subcutaneous wall thoracic abscess. However, in a large study about the epidemiology of candidemia in the setting of intensive care unit (ICU), Galván B et al. [10], showed a low incidence (3%) of this complication in the context of HIV infection. Treatment of skin and subcutaneous lesions due to Candida albicans includes the surgical excision with drainage, systemic antifungal therapy and, eventually, the removal of devices or intravenous catheters. Antifungal therapy based on azolic drugs is the best option for cutaneous and subcutaneous candidiasis. Fluconazole is a fungistatic drug against Candida species and, used in doses of 400 mg daily, appears to be an adequate treatment as we could see in this patient. This case makes evident the importance of a high index of suspicion and the need to culture all samples obtained from subcutaneous abscess to probe the definitive diagnosis of Candida albicans.
References
- Nucci M, QueirozTelles F, Alvarado-Matute T, Tiraboschi IN, Cortes J, et al. (2013) Epidemiology of candidemia in Latin America: A laboratory-based survey. PLoS ONE 8: e59373.
- Tuon FF, Nicodemo AC (2006) Candida albicans skin abscess. Rev Inst Med Trop Sao Paulo 48: 301-302.
- Collingon PJ, Sorell TC (1983) Disseminated candidiasis evidence of a distinctive syndrome in heroin abusers. Brit Med J 287: 861-862.
- Manfredi R, Mazzoni A, Nanetti A, Mastroianni A, Coronado OV, et al. (1997) Isolated subcutaneous candidal abscess and HIV disease. Br J Dermatol 136: 647-649.
- Mazumdar PK, Marks MI (1975) Candida albicans infections in hospitalized children: a survey of predisposing factors. Clin Pediat (Phila.) 14: 123-129.
- Corti M, Solari R, De Carolis L, Cangelosi D, Arechavala A, et al. (2013) Candida parapsilosis meningitis in a patient with AIDS. Report of a case and review of the literature. Rev Iberoam Micol30: 122-124.
- Kuhn DM, Chandra J, Mukherjee PK, Ghannoum MA (2002) Comparison of biofilms formed by Candida albicans and Candida parapsilosis on bioprosthetic surfaces. Infect Immun 70: 878-888.
- Yampolsky C, Corti M, Negroni R (2010) Fungal cerebral abscess in a diabetic patient successfully treated with surgery followed by prolonged antifungal therapy. Rev Iberoam Micol 27: 6-9.
- Chapman SW, Daniel CR (1994) Cutaneous manifestations of fungal infections. Infect Dis Clin North Am 8: 879-910.
- Galván B, Mariscal F (2006) Epidemiology of candidemia in ICU. Rev Iberoam Micol 23: 12-15.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences